By Darby Kendall
For Ignite Magazine
Illustrations by Chelsea Pham/OHSU Foundation
Twelve years ago, Phil and Penny Knight issued an historic philanthropic challenge to the OHSU Knight Cancer Institute: raise $500 million within two years, and they would match it — creating a $1 billion investment to advance cancer research. As Phil said when delivering the challenge: Is there a higher calling than curing cancer?
In 2015, with the help of thousands of donors, the OHSU Foundation successfully raised $500 million, securing the Knights’ matching gift. The Knight Cancer Challenge became the largest documented challenge pledge to succeed, and the milestone brought with it a renewed hope toward ending cancer as we know it. A significant part of that hope was a fresh focus on the early detection of lethal cancers — one of the biggest unmet needs in cancer care at the time.
One year later, the creation of the Knight Cancer Institute’s Cancer Early Detection Advanced Research Center (CEDAR) marked the beginning of a new era in precision early detection. CEDAR was founded with a single mission: detect and stop lethal cancers at the earliest stage because early detection saves lives. In the years since its opening, the center has employed 174 professionals, conducted over 290 philanthropy-funded research projects and authored more than 170 peer-reviewed publications.
Multidisciplinary scientific collaboration is an essential component of CEDAR’s success. Fulfilling the promise of the Knight Cancer Challenge, the Knight Cancer Institute and CEDAR have recruited, organized and empowered dozens of brilliant, passionate people from radically different scientific backgrounds to come together around a common goal and solve complex problems. From bioprinting human tissue to utilizing super-resolution microscopy, these scientists are bringing early cancer detection into a new era.
Here are just a few of the incredible people at the Knight Cancer Institute working to transform cancer science, early detection and the future of patient care.
Ece Ekşi, Ph.D.
Assistant professor at CEDAR and the Division of Oncological Sciences
Ekşi’s research explores how the nervous system communicates with tumors, particularly in prostate and pancreatic cancers.
Luiz Bertassoni, D.D.S., Ph.D.
Founding director of the Knight Cancer Precision Biofabrication Hub, professor at the Division of Oncological Sciences and co-section head for Discovery and Translational Oncology
Bertassoni leads a multidisciplinary research group working on several groundbreaking uses of biofabrication to study cancer, including 3D bioprinting, organs-on-a-chip, and stem cell regenerative medicine.
Thuy Ngo, Ph.D.
Associate professor in the Department of Molecular and Medical Genetics
Ngo’s work involves analyzing blood samples for signs of early disease, aiming to detect signals from the body that mark transitions from healthy to cancerous states.
Carolyn Schutt Ibsen, Ph.D.
Assistant professor at CEDAR and the Department of Biomedical Engineering
Using ultrasound waves, Schutt Ibsen is able to remotely control the behavior of cells deep within the tissues she engineers, allowing for precise genetic changes that don’t disrupt the tissue structure.

Joshua Moreau, Ph.D.
Assistant professor at CEDAR, the Division of Oncological Sciences, Department of Dermatology, and Department of Cell, Developmental and Cancer Biology
As an immunologist, Moreau focuses on understanding adaptive immune function, particularly in peripheral tissues like the skin. Moreau’s lab has found promising research on a type of immune cell, the memory B cell, that could act as a therapeutic target for cancer.
Cristiane Miranda Franca, D.D.S., Ph.D.
Assistant professor at CEDAR and the School of Dentistry
Franca is a core faculty member in the Knight Cancer Precision Biofabrication Hub, recreating environments on-a-chip, such as mucosa and lymphatic vasculature, to study epithelial cancer development and invasion.


Matthew Rames, Ph.D.
Research engineer at CEDAR
Rames’ work with microscopy and imaging technologies allows him to look at cellular structures like mitochondria and the ways they’re impacted by cancer.
Xubo Song, Ph.D.
Scientific co-director of the Center for Biomedical Data Science and professor at the Division of Oncological Sciences, the Department of Medical Informatics and Clinical Epidemiology and the Department of Biomedical Engineering
Song specializes in machine learning and AI, applying them to biomedical data, especially images focusing on cancer research.

“My research cannot exist in a silo. It requires collaboration between engineers and computational biologists, pathologists and radiologists and geneticists. The Knight Cancer Institute and CEDAR provide that collaboration for innovative research.” – Ece Ekşi
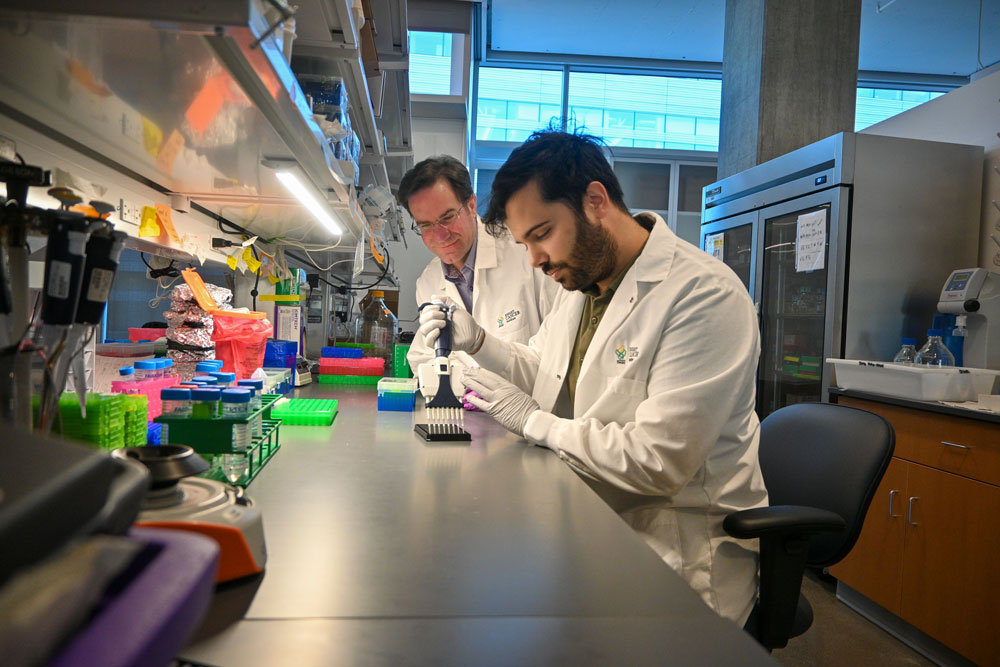
Jared Fischer, Ph.D., left, and Jose Luis Montoya Mira, Ph.D., cancer researchers at OHSU, have developed PAC-MANN, a test that uses a small blood sample to detect changes in protease activity, a key indicator of the most common and deadliest form of pancreatic cancer. (OHSU/Christine Torres Hicks)
Shared ideas yield innovative results
A new blood test developed by CEDAR researchers Jose Luis Montoya Mira, Ph.D., and Jared Fischer, Ph.D., identifies hard-to-detect pancreatic cancer with 85% accuracy. The test could help doctors identify pancreatic cancer earlier, leading to improved survival rates for patients.
“Our test could be used for people at high risk of pancreatic cancer, which is not targeted by current tests,” Montoya said. “It allows for a more robust and less invasive screening, unlike an endoscopic ultrasound and other liquid biopsy tests that require large volumes of blood, thus allowing our test to be performed more frequently for earlier detection.”
Pancreatic cancer is often diagnosed at an advanced stage when treatment options are limited. Current tests are good at indicating prognosis but aren’t sensitive enough for early-stage detection. Montoya and Fischer led the development of a test that requires a small blood sample to detect changes in protease activity, a key indicator of the most common and deadly form of pancreatic cancer.
The researchers created a non-invasive test using blood samples from 350 patients from OHSU’s Brenden-Colson Center for Pancreatic Care and CEDAR. While this test is not yet available to the public, there are plans for more trials, specifically an investigator-initiated trial in patients at high risk of developing pancreatic cancer.
“This test isn’t just about detection — it could also help us measure how well treatments are working and guide therapeutic options,” Fischer said. “If we can track a patient’s response to therapy in real-time, we can make better treatment decisions and improve outcomes.”
Both Montoya and Fischer operate within CEDAR as cross-collaborators with other scientists, a mainstay of the center’s goal to bring diverse expertise and ideas together. It is minds like theirs that are working to transform cancer research, early detection and the future of fighting this disease.




