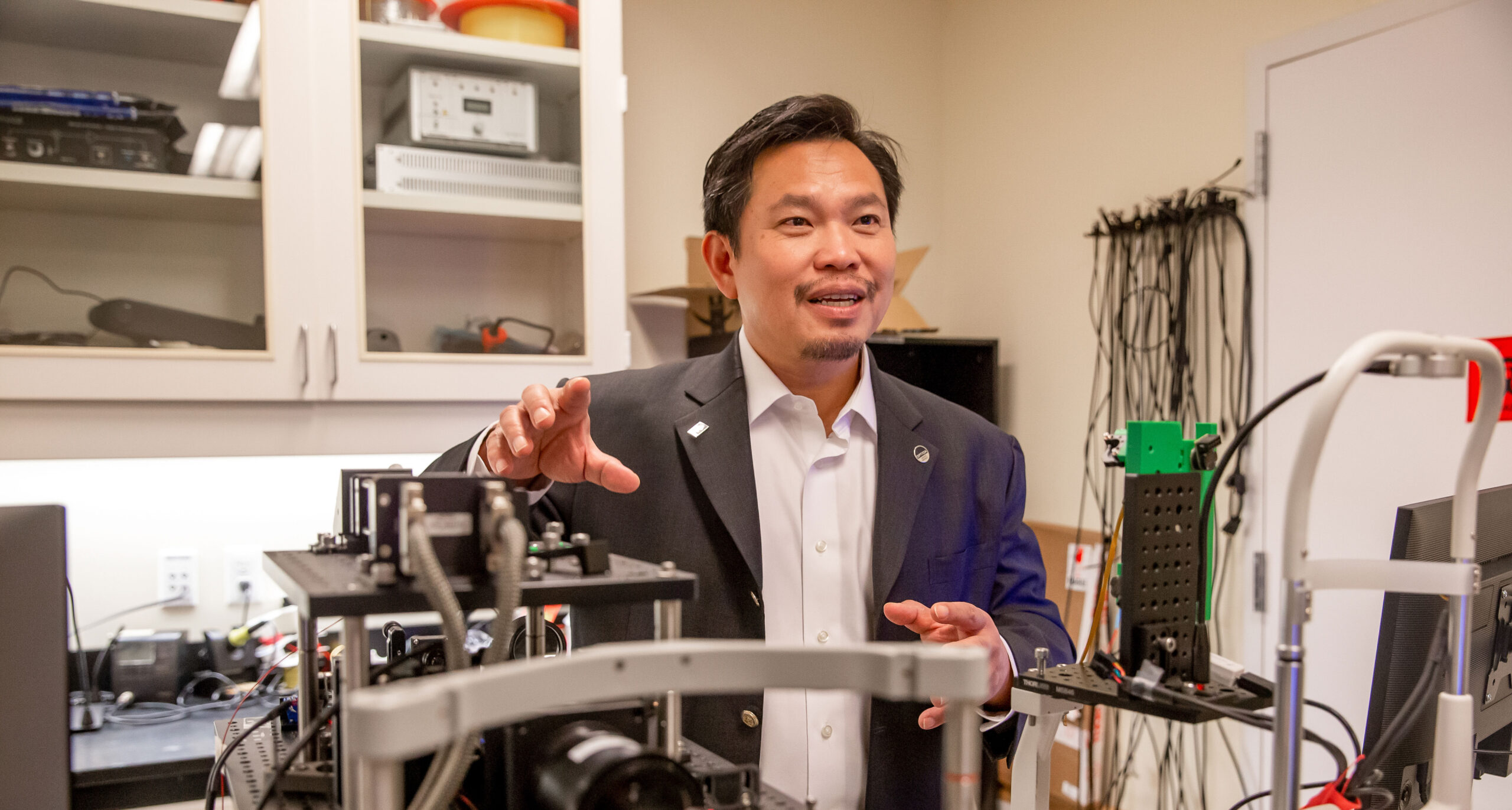
David Huang reflects on his optical imaging discovery — and how graduate research made it possible.
By Darby Kendall
For Ignite Magazine
Fresh eyes can usher in new ways of understanding. That was certainly the case when David Huang, M.D., Ph.D., pursued an imaging project as a graduate student in a laser laboratory at MIT. That project transformed into the novel invention of optical coherence tomography (OCT), a technology that has since revolutionized the field of ophthalmology. OCT has been so influential that Huang and his co-inventors James G. Fujimoto, Ph.D., and Eric A. Swanson, M.S., received the 2023 Lasker-DeBakey Clinical Medical Research Award, otherwise known as “America’s Nobel.”
Trusting the process
Huang started his graduate studies entirely outside the field of ophthalmology. At the Harvard-MIT Program in Health Sciences and Technology, Huang first worked in tissue mechanics to generate artificial ligaments, but a gut feeling told him to explore other fields. Intrigued by the potential applications of lasers in medicine, Huang made the switch to optics.
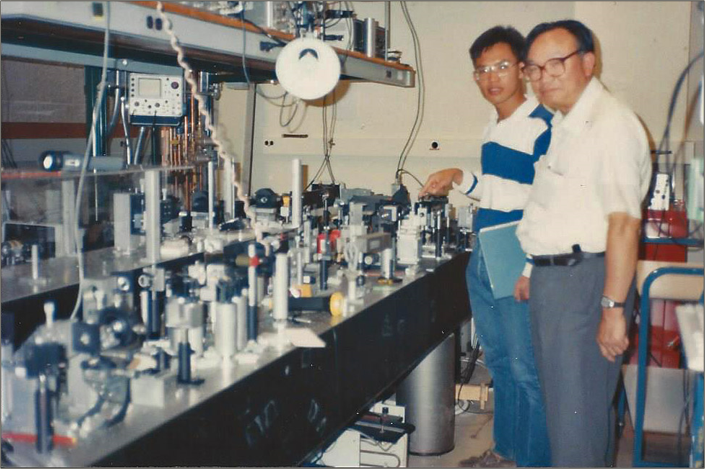
In 1990, the idea for OCT began to take shape in Huang’s mind. Though OCT is now the gold standard of ocular imaging, the method was originally an exploratory project assigned to Huang by Fujimoto, Huang’s Ph.D. thesis advisor. “OCT started as a small side project in this large laser laboratory. My setup with the interferometer occupied a tiny corner of this optical table,” Huang remembered. An interferometer is a tool that analyzes the interaction between two light waves. In Huang’s case, he was using it to measure the time-of-flight of light reflected from biological tissue.
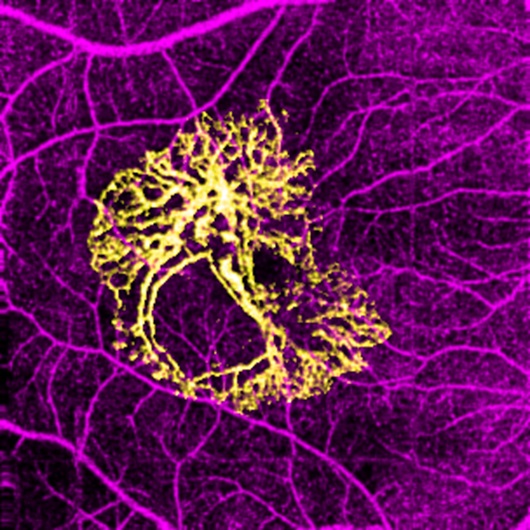
Serendipitously for Huang and the field of ophthalmology, Huang happened to begin this investigation by measuring light reflected in the eye, and he soon ran into unexpected findings that led to a breakthrough. “I found that it was not easy to measure retinal thickness. So, I scanned the beam of light laterally to form a cross-sectional image. The image beautifully revealed many layers inside the retina, a structure that is as thin as a strand of hair.”
Huang and his team had invented a new technology that could see 10-100 times finer detail than other imaging modalities. They got to work building the necessary technology to translate this discovery into a clinical instrument. They published the first OCT images of the retina and other tissues in 1991 in the journal Science. That article has now been cited more than 18,000 times.
Despite OCT’s revolutionary imaging capabilities, there was still pushback from others in the field.
“Some people were in love with it right away; they could see the potential even though the images from first-generation OCT systems were grainy,” Huang said in a recent episode of the Experts InSight podcast, hosted by Benjamin K. Young, M.D., assistant professor of ophthalmology in the OHSU School of Medicine. “In the other camp were people who weren’t impressed with the images. They thought this was a tool to make people forget the art of detailed retinal examination … By 2002 [when high-quality OCT imaging became clinically available], I don’t think anyone could reasonably say that their retinal examination could produce diagnoses as accurate as retinal OCT.”
A transformational impact
OCT is now widely accepted and used in more than 40 million imaging procedures yearly to diagnose and treat the leading causes of blindness. The imaging method also helps physicians determine when to provide injections for wet macular degeneration, which often leads to fewer injections and reduces cost. Huang and his colleagues reported that between 2008 and 2015, it saved Medicare and its patients a combined $11.2 billion.

Beyond monetary benefits, the ease of OCT’s use aids the Casey Eye Institute’s goal to eliminate preventable blindness in Oregon and beyond.
“The reason OCT is used so much in ophthalmology is because its noninvasive, fast and inexpensive,” Huang said. “OCT is perfect for our outreach mission because it’s portable and economical, so we can put OCT systems in rural communities, use them to detect eye diseases and make referrals to eye specialists when needed.”
Looking to the future of OCT imaging, there is great potential for its applications with diagnoses in other fields, including dermatology and gastroenterology. Reflecting on how far OCT has come, Huang is grateful for his chance to make a major contribution to medical science and is excited for what’s to come. “I think we’ll see OCT used more in other tissue structures in the future because of the continual technology improvement,” he told Young. “Being able to see things that were invisible before can be very powerful.”
The vital importance of early career scientists
Early career researchers bring new ideas, fresh perspectives, energy and enthusiasm to their fields. Huang brought curiosity and innovation to the field of ophthalmology — and it transformed the entire future of optical imaging.
Huang agrees with the power of graduate research. “I think a graduate student has the enviable freedom to devote one’s time to learn a wide variety of subjects and experiment with ideas within the constraints of the resources provided by the mentor’s laboratory,” he said.
Graduate students power the research engine at academic medical centers such as OHSU. It’s also a demanding role. Doctoral students, in particular, must immerse themselves fully in learning the fundamentals of their discipline while also working long hours in the laboratories of their faculty mentors. They are the ones who most often perform the painstaking, day-to-day bench science at the foundation of every major breakthrough.
Yet as Huang himself experienced, this demanding regimen of study and work lengthens the time it takes even the most exceptional students to complete their degree requirements. “When my father visited me at MIT during my thesis research, he asked why it was taking me so long to finish my degrees,” Huang said. “Neither of us were sure it was worth taking an extra four research years to the already lengthy four-year medical school curriculum. But, in retrospect, those years yielded tremendous benefits to myself and to medicine.”
The average M.D.-Ph.D. student needs seven to eight years to complete the program, with a growing number taking 10 or more years to graduate. Too many promising future leaders are forced to quit due to financial strain alone. Private philanthropic funding and scholarships make a substantial impact in graduate research — keeping these bright, fresh minds within their fields of study.
Because the reality is: You never know when the next OCT might happen.
When graduate research students are encouraged to follow their instincts — and have the financial stability to do so — scientific breakthroughs are made possible.