By Darby Kendall
For Ignite Magazine
It’s often said that sleep is the best medicine, and Miranda Lim, M.D., Ph.D., is on a mission to prove the proverb right.
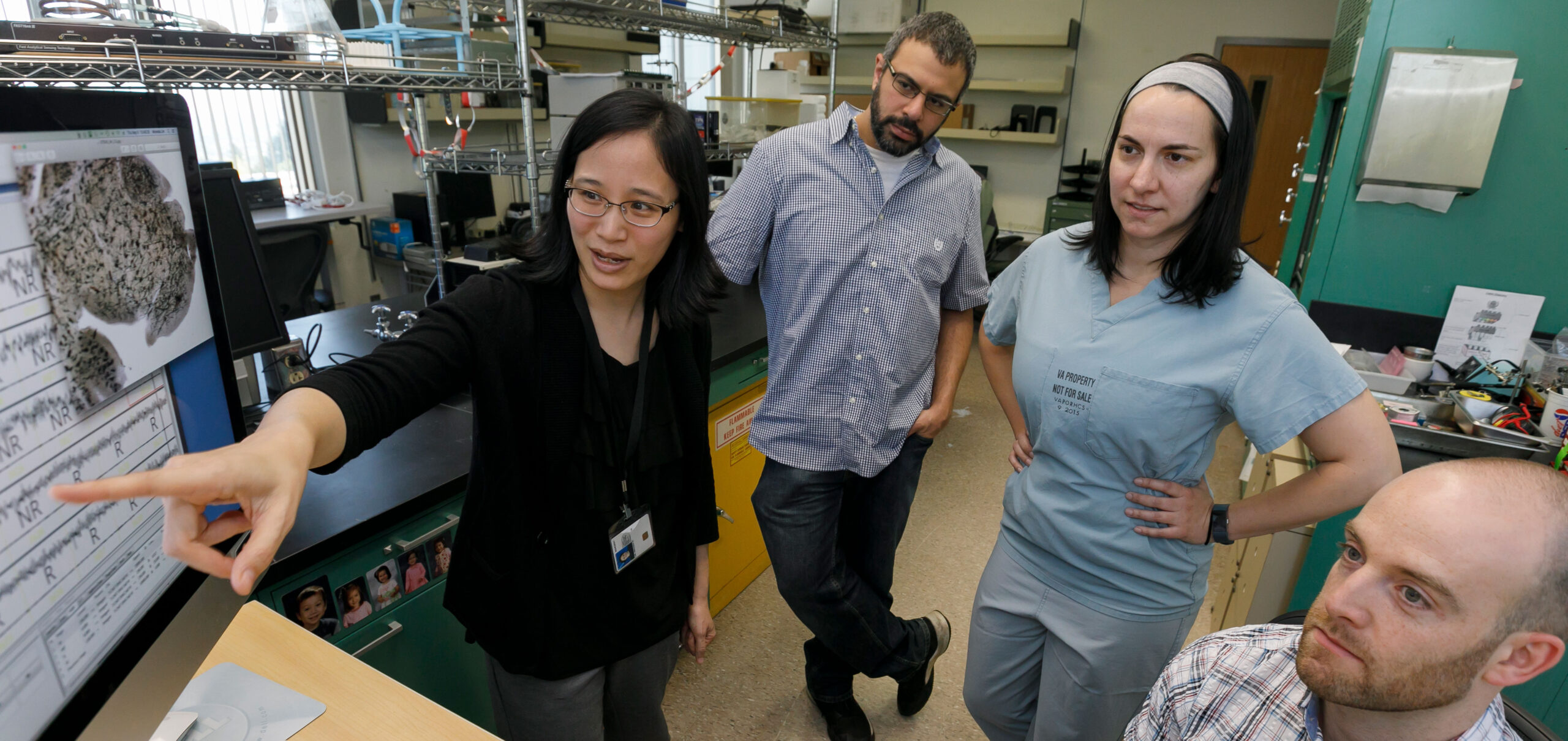
A good night’s rest can make all the difference in someone’s day, but how much shut-eye we get also has powerful implications when it comes to brain health. Lim, a physician-scientist and co-director of the OHSU Layton Aging and Alzheimer’s Disease Research Center and the Sleep & Health Applied Research Program (SHARP Lab), studies sleep in relation to a variety of disorders to get to the bottom of how it impacts the brain.
“Every single person has a personal story about sleep, and it makes such a big difference to our quality of life, our outlook, our relationships, the things that make us most human and that we value,” Lim said. “Understanding why sleep is important and uncovering the biology, that’s what drives me most as a scientist and as a neurologist.”
The study of sleep in relation to dementia is a relatively new field, with the science on it growing only over the past 15 years. A revelation during Lim’s time as a neurology resident at Washington University in St. Louis inspired her to pursue the subject.
“We ended up making the first discovery that sleep deprivation accelerates the pathology that you see in the brains of Alzheimer’s patients. There’s something about the biology of sleep that probably helps to wash the brain and inhibit the aggregation of these toxic proteins that can cause memory loss, and even Parkinson’s and motor problems,” Lim explained. “I was hooked on sleep from that point onward.”
“It turns out, over 90% of people with this disorder end up developing Parkinson’s disease. This might be the earliest disease manifestation before we know someone’s going to develop it, and it’s an amazing opportunity to intervene.”
At the SHARP Lab, Lim covers a broad range of neurological topics with her research, breaking down her work primarily into three stages of life. She believes that in order to truly uncover the function of sleep, one has to understand its function across the lifespan. In infancy and childhood, sleep can help shape proper brain development, and lack of sleep may affect the likelihood of developing autism — “it turns out that children with autism have significantly reduced amounts of rapid eye movement (REM) sleep. There’s something really important about the function of REM sleep early in life in shaping social development and how the brain grows.” In her studies on young and middle-aged adults, Lim examines risk factors that predict neurodegeneration, such as chronic impaired sleep due to concussion or post-traumatic stress disorder, which are known risk factors for dementia. For older adults, Lim studies the brain and sleep patterns in relation to Alzheimer’s and Parkinson’s disease.
Discovering a precursor to Parkinson’s disease
One significant dimension to Lim’s work is her partnership with the Portland VA Medical Center, where she serves as a neurologist evaluating and treating veterans with sleep disorders. Lim noticed an unusually high percentage of veterans with REM sleep behavior disorder, also known as RBD, when people physically and vocally act out their dreams, sometimes causing severe injuries to themselves or their bed partners. Nearly 5% of all veterans in her sleep lab were found to have RBD, and the statistic jumped up to 20% for veterans who sustained a traumatic brain injury with post-traumatic stress disorder as well. Lim was intrigued by the high numbers of RBD she was seeing in her clinic, because, after reviewing other studies, she learned it was tied to neurodegenerative conditions.
“It turns out, over 90% of people with this disorder end up developing Parkinson’s disease,” Lim said. “This might be the earliest disease manifestation before we know someone’s going to develop it, and it’s an amazing opportunity to intervene.”
This discovery provides a unique opportunity to help patients earlier, before the onset of Parkinson’s, when treatments are more likely to be effective. Civilian populations are affected by RBD as well, with up to 1 in 100 people impacted by the disorder, so Lim’s research could have wide-reaching impact in early intervention with Parkinson’s disease.
Treating dementia with deep sleep
Chronic sleep deprivation can greatly affect the aging brain. When we sleep, the brain flushes away beta amyloid, a protein that clusters together to form Alzheimer’s-causing plaques between nerve cells in the brain. The less sleep someone gets, the greater the buildup of beta amyloid they’re likely to have, increasing their chance of developing dementia later in life.
Though the link poses concerns for those who struggle with sleep, Lim looks at the discovery with optimism — those who are at risk for dementia can be screened before signs of Alzheimer’s ever arise, and their sleep quality can be preventatively improved. “If sleep is something that can help mitigate risk for Alzheimer’s and Parkinson’s, then we should be really paying attention to it,” Lim emphasized.
“I think that our society places a lot of emphasis on people who are young. There is this tendency to ignore or forget people as they get older, and I think that does us a disservice,” Lim said. “As we get older, we relearn different perspectives and ways of dealing with things that can only come with age. I live to support aging in a way where people can still achieve all the things they want to achieve.”
Groundbreaking research empowered by philanthropy
An essential part of what keeps Lim’s work going is the philanthropic support of the Layton Aging and Alzheimer’s Disease Research Center. The additional funding through private philanthropy allows expanded sleep data collection and strengthens their efforts to serve diverse communities, a priority for Lim, who is deeply committed to advancing DEI.
“Recent philanthropy has allowed us to support important outreach efforts to our local community, in particular to historically underrepresented and marginalized groups in Oregon,” Lim said. “Philanthropy has been such a key catalyst for our work in the center. It allows us to do cutting-edge research that is high-risk, high-reward, early in developmental stages — true instruments for change.”
Having co-led the Layton Aging and Alzheimer’s Disease Research Center for over a year now, Lim is energized by the progress sleep science has in store. She envisions a future where sleep research not only deepens our understanding of aging, but also transforms the way we approach dementia prevention and cognitive health.
“I’m excited for the vision for the next five years to include more about sleep health and understanding how sleep fits into this overall picture of healthy aging and cognition, including risk for dementia,” Lim said. “I think there’s a lot to be done. It would be wonderful to tie all those pieces together and tell a new story that has sleep as a driving force for our health and well-being.”
On Jan. 14, 2025, President Joe Biden recognized Miranda Lim among recipients of the Presidential Early Career Award for Scientists and Engineers.
Watch a KGW News story on Dr. Lim’s work from Feb. 5, 2025.