“If only we had caught it earlier.” It’s a tragically familiar reaction when a patient receives a grave diagnosis. Our society’s most dreaded and debilitating health conditions — cancer, heart disease, dementia, blindness — often take root years before they cause troublesome outward symptoms. Timely detection of the earliest signs of nascent disease can save precious time, allowing physicians to take quick action to solve problems before they start.
Although the life-saving promise of early detection is well-established, the needle-in-a-haystack search for clinically relevant early-stage disease indicators has been stymied by limitations in current screening technologies. But that’s beginning to change. With the support of its donors, OHSU is at the forefront of a growing global community of scientists and clinicians developing a new generation of more precise, patient-friendly tools for early detection of cancer and other serious diseases.
Better Tools for a Closer Look
Today’s routine screening methods for conditions such as breast, colon or prostate cancer have saved many lives. They can and do help medical teams pinpoint signs of disease while there is still time to take decisive action. But not always. Even the best of today’s standard tests are not sensitive enough to find and precisely characterize the molecular-level precursors of disease before they develop the capability to threaten a patient’s health. Consequently, too many patients are diagnosed only after their disease has progressed too far to be effectively treated.
At OHSU, researchers envision a very different approach to disease detection — one that is simple, painless and cheap, and that catches life-threatening diseases before they can cause problems for patients. Imagine a future when women’s annual breast cancer checks are achieved as part of a routine blood draw. When a noninvasive vision test might also reveal invisible warning signs of heart disease or diabetes. Or when a neurologist can conclusively diagnose Alzheimer’s disease while there is still time to slow its progression.
That future is based on the development of clinical tools and techniques that catch signs of diseases before they start so doctors can stop them before they cause irrevocable harm. Early detection researchers are focused on finding and characterizing more nascent indicators of disease than previously imaginable. In the process, they are opening the door to a future of precision medicine — where treatments are designed to address the unique biological drivers of each patient’s illness.
“Over 80% of patients with pancreatic cancer have the disease detected too late to even have a chance at curative multidisciplinary therapy.”
Brett Sheppard, M.D., FACS
This future is coming into reach, but it has not been easy. The pace of progress in early detection technology has been glacial, in part because federal research funding prioritizes the next blockbuster drug. However, recent and dramatic technological advances in genomic sequencing, supercomputing and high-resolution microscopes are creating exciting new possibilities in early detection research. Powerful image processing technologies are giving researchers a sub-molecular glimpse into the inner workings of human cells and tissues. Combined with modern techniques of DNA analysis, machine learning and artificial intelligence, these technologies are helping them learn to recognize and understand the early markers of disease progression, and to imagine creative ways to measure and treat it before it becomes lethal. Private support from individual philanthropists, corporations and private foundations has enabled many of the vital discoveries and developments that are accelerating the pace of progress in early detection.

Donor-Driven Discovery
Philanthropic support has helped OHSU develop unsurpassed expertise in this emerging field over the past 20 years and continues to play a vital role in moving promising ideas from the laboratory into clinical settings. Through the landmark Oregon Opportunity campaign from 2000 to 2007, OHSU enlisted donors and the state of Oregon to raise more than $500 million in private and public support to elevate OHSU’s capacity for bioscience innovation and discovery. Donor dollars enabled OHSU to recruit exceptional researchers and construct the Hildegard Lamfrom Biomedical Research Building, providing state-of-the-art laboratory space and key enabling technologies in early detection such as advanced magnetic resonance imaging (MRI), bioinformatics, next-generation sequencing and biomedical engineering.
And that was just the beginning. OHSU drew international attention to the promise of early detection in 2013 through the Knight Cancer Challenge fundraising campaign, an unprecedented — and as yet unsurpassed — two-year philanthropic effort that raised $1 billion for cancer research at OHSU. The tangible result of this headline-making drive was two-fold: the seven-story, 320,000-square-foot Knight Cancer Research Building (KCRB) on OHSU’s South Waterfront Campus and the creation of the building’s principal tenant, the OHSU Knight Cancer Institute’s Cancer Early Detection Advanced Research Center (CEDAR).
CEDAR’s mission is to accelerate progress in the early detection of cancer — developing new, less-invasive tests to spot emerging tumors at the most treatable stage and exploring new ways to differentiate among harmless, slow-growing or potentially lethal tumors. CEDAR actively recruits exceptionally innovative scientists to join its ranks. This unique think tank within the Knight Cancer Institute is a bastion of multidisciplinary team science where researchers at all levels of experience contribute their boldest ideas for high-risk/high-reward projects.
“We are at a pivotal scientific moment as many new approaches, such as fluid biopsies for detection and immunotherapies for treatment, are emerging,” said CEDAR Director Sadik Esener, Ph.D., the Wendt Family Endowed Chair in Early Cancer Detection and professor of medicine in the OHSU School of Medicine. “We have built an outstanding team that leveraged the pioneering work that was already underway at OHSU, and rapidly established a global set of collaborations with industry and other leading academic institutions to play a pivotal international role in this area.”
Esener’s team is working to shorten the time it takes to move a great idea from the laboratory into the clinical setting. Using philanthropic dollars to emulate the fast “go/no go” decision-making approach of a private company, CEDAR puts new ideas to the test in rigorous proof-of-concept studies that rapidly determine which ones have potential and which do not. The best ideas are fast-tracked for further development while less successful projects are sent back to the drawing board or discontinued. The goal is to identify and invest in early detection technologies that can then be transferred to a spin-off company or industry partner for further development and regulatory approval — part of CEDAR’s mission to support the growth of Oregon’s bioscience business sector.
Synthetic Bones, Real Solutions
Many CEDAR-driven ideas are already poised for impact. Take, for example, the “bone in a dish.” CEDAR member Luiz Bertassoni, D.D.S., Ph.D., and coworkers developed an engineered material that precisely replicates the structure and biological functioning of human bone tissue. Grown in a Petri dish, this synthetic copy has all the features of real, living bone — including a 3D mineral structure populated with bone cells, nerve cells and endothelial cells that organize themselves into functioning blood vessels. Bertassoni’s team uses the “bone in a dish” as an experimental model to answer important questions in early detection research.
“With this model system, you can start asking questions about how bone cells attract different types of cancers, how cancer cells move into bone and how bone takes part in the regulation of marrow function,” said Bertassoni, who is an associate professor of restorative dentistry in the OHSU School of Dentistry.
This work and similar projects inspired the launch of the Knight Cancer Precision Biofabrication Hub in the KCRB where, under Bertassoni’s leadership, researchers will expand on tissue engineering technologies to build complex models of early cancers for research. The research has also led to the creation of a spin-off company, Humarrow, Inc., that hopes to commercialize a technology for generating exact, living copies of a cancer patient’s unique bone marrow cells in an experimental model for testing leukemia therapies. By trying out different drug combinations on this synthetic marrow before giving them to the patient, doctors can find the optimal treatment for the patient without losing critical response time to trial and error, which often happens in oncology.
Upgrading the Annual Blood Draw
Another CEDAR member, Thuy Ngo, Ph.D., an assistant professor of molecular and medical genetics in the OHSU School of Medicine, has led the development of a promising blood test designed to reveal the early signs of two lethal cancers — liver cancer and multiple myeloma — in people known to be at risk for these diseases. The test looks for molecules called messenger RNA — or mRNA — which carry instructions from genes. These structures routinely “escape” from cells and circulate in the blood.
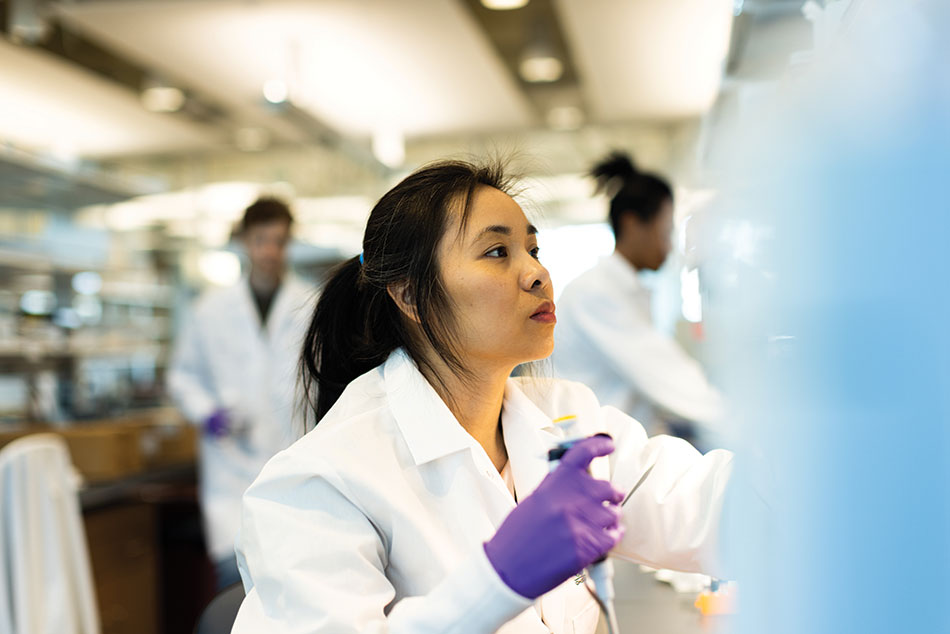
If a cancer cell is present, those escaped mRNA will carry evidence of genetic instructions to create more cancerous cells.
Until recently, scientists had no way to capture this evidence, Ngo said. “A few years ago, not many people believed cell-free messenger RNA could be reliably detected in the blood because [mRNA] is prone to degradation. We found a way to handle it, and we are among the first to apply it in cancer and precancer early detection.”
The research lays the foundation for developing inexpensive assays. “You don’t need any fancy equipment for doing this,” Ngo said. “Any central lab with standard equipment can do the work.”
CEDAR’s scientific reach extends beyond the basic science lab and into the community, through clinical trials and population-based research. On the strength of the Knight Cancer Institute’s expertise and leadership in early detection, the institution was selected by health care innovator GRAIL, Inc., as one of only five U.S. test sites for a groundbreaking clinical study of an early detection blood test for multiple cancers (see story on page 12). Building on this expertise, CEDAR is launching new clinical trials with GRAIL and additional industry partners focused on either multicancer tests or disease-specific blood tests.


Jumpstarting Pancreatic Care
Beyond CEDAR, other researchers across OHSU are also seeking new approaches to early detection. For example, pancreatic cancer is a relatively rare disease, yet it has one of the highest mortality rates of all cancers. Why? Because it is almost always detected at a late stage. Pancreatic tumors can develop unnoticed for years because they cause no noticeable symptoms until they become dangerous and begin to spread to other organs.
“Over 80% of patients with pancreatic cancer have the disease detected too late to even have a chance at curative multidisciplinary therapy,” said pancreatic surgeon Brett Sheppard, M.D., FACS, co-director of OHSU’s Brenden-Colson Center for Pancreatic Care, the William E. Colson Chair of Pancreatic Disease Research and a professor and vice chair of clinical operations and quality for the Department of Surgery in the OHSU School of Medicine. “Our center is deep in research protocols to develop new blood- and saliva-based biomarkers to help detect pancreatic cancer earlier.”
The perennial lack of progress in diagnosing and treating pancreatic cancer, pancreatitis and other pancreatic diseases inspired Norman and Linda Brenden and the Colson Family Foundation to join philanthropic forces in 2013 with a $25 million gift to establish the Center, which is co-led by Rosalie Sears, Ph.D., a professor of molecular and medical genetics in the OHSU School of Medicine and the Krista L. Lake Chair in Cancer Research. Since then, the Brendens have continued to support the center with gifts of $5 million, $15 million and, most recently, $10 million.
OHSU’s robust program of early detection research isn’t exclusive to cancer. Groups across the university are exploring innovative new ways to find and address other health problems before they start.
The Eyes Have It
Harnessing the power of advanced artificial intelligence and high-resolution ocular imaging, OHSU’s Casey Eye Institute is poised to transform the early detection and treatment of eye disease — and eventually other systemic health problems.
Optical coherence tomography (OCT), a critical ocular imaging technique developed by Casey Associate Director David Huang, M.D., Ph.D., is today’s most effective method for capturing ultrahigh-resolution, 3D images of the retina. Ophthalmologists use OCT to diagnose many vision-threatening eye diseases, including the three leading causes of blindness: age-related macular degeneration (AMD), diabetic retinopathy and glaucoma. This technology’s ongoing development, when combined with breakthroughs in artificial intelligence to recognize disease patterns in these images, is giving rise to the emerging field of “oculomics.”
“The technologies we have developed can detect common eye diseases with exquisite sensitivity,” Huang said. “But they can also be used to detect retinal amyloid plaques in Alzheimer’s disease or changes in retinal blood flow due to cardiovascular diseases. We are ready to expand the reach of these technologies to a broader population.” Huang is a professor of ophthalmology and biomedical engineering as well as the Martha and Eddie Peterson Professor of Ophthalmology in the OHSU School of Medicine.
In the decades to come, it is likely that oculomics will make it possible to catch the early warning signs of multiple sclerosis, Alzheimer’s disease, stroke, cardiovascular disease, diabetes and many other disorders by examining the eye.
The concept of oculomics as a multipurpose diagnostic method is in its infancy and will require much more study before it is ready for routine clinical use. In the meantime, the underlying OCT technologies are making significant inroads against the most complex, challenging forms of AMD.
Macular degeneration manifests itself in two distinct ways: the “wet” type, which is caused by the growth of abnormal blood vessels, and the “dry” type, which arises when retinal cells begin to atrophy (waste away). OCT’s ability to visualize the processes behind wet AMD has enabled the development of a number of new treatments to stop vision loss. Going forward, the challenge is to develop new OCT methods for the less-detectable and harder-to-treat dry form.
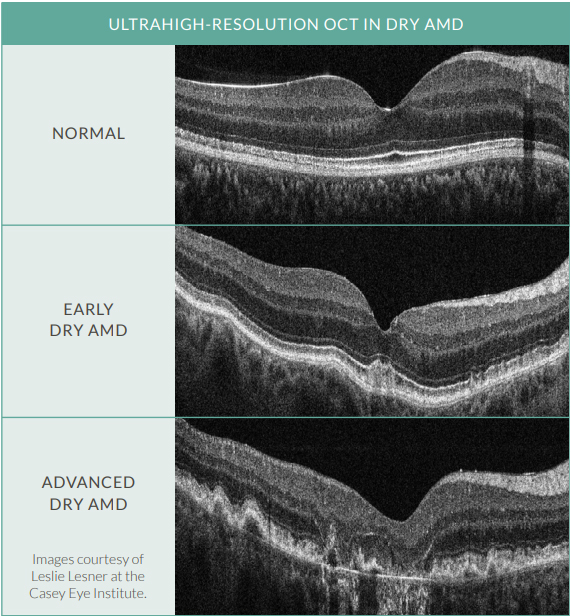
“In dry AMD, our advances in imaging have made it possible to visualize the degeneration of the layers in the retina before vision is affected. Detecting these changes is key to early diagnosis, as well as assessing the effectiveness of potential new drugs to treat dry AMD,” said Huang, who holds the Martha and Eddie Peterson Professorship in Ophthalmology. His team continues to develop new OCT techniques that, combined with high-performance computing, will help patients retain the gift of sight throughout their lives.
Seeking Clues to Brain Disorders
Many OHSU researchers are striving to improve existing technologies. But some teams seek to create diagnostic tools for diseases that have defied early detection for generations. In the case of Alzheimer’s disease — the nation’s seventh leading cause of death and the most feared disease among older Americans — a conclusive diagnosis requires a post-mortem examination of brain tissue. Although there is no cure, studies show early intervention can significantly slow progression and improve the quality of life for both patients and caregivers. The Alzheimer’s Association projects the disease will impact 12.7 million people over the age of 65 by 2050, underscoring the urgency to confront this growing public health challenge.
Julie A. Saugstad, Ph.D., a professor of anesthesiology and perioperative medicine and of molecular and medical genetics in the OHSU School of Medicine, is leading a multidisciplinary team studying novel biomarkers that could predict the onset of Alzheimer’s and also help distinguish the disease from other forms of dementia. In collaboration with physician-researcher Joseph Quinn, M.D., holder of the Wayne and Sandra Ericksen Professorship for Neurodegenerative Research and director of the Parkinson Center and Movement Disorders Program in the OHSU School of Medicine, the team focuses on the possible use of microRNAs as a patient-friendly test for early Alzheimer’s indicators. MicroRNAs are structures that work together with messenger RNA to regulate gene expression. Though existing primarily within cells, messenger RNA, microRNAs and other non-coding RNAs have been detected in most body fluids. MicroRNAs found in cerebral spinal fluid may hold clues about the abnormal chain of events in the central nervous system that give rise to Alzheimer’s and other dementias. The team is focusing on identifying and evaluating a number of microRNA-based biomarkers through basic research and clinical trials.
A Philanthropy-Fueled Revolution
These dedicated teams, novel studies and game-changing discoveries are only a portion of OHSU’s programs in early detection research. Though there are a variety of approaches and aims, each project demonstrates the power of philanthropy to open new doors in biomedical research. Whether by creating endowed chairs and professorships that help OHSU retain and attract top research talent; supporting the acquisition of state-of-the-art research equipment; establishing dedicated research centers; funding innovative research; or providing financial aid for students and trainees; OHSU donors are closing the innovation gap and opening up limitless life-saving possibilities.




